With winter just around the corner, NHS Humber and North Yorkshire Health and Care Partnership are advising their residents on the best ways to stay well during the cold weather.
Ordering repeat prescriptions
Residents in North Lincolnshire who are on repeat medication are being encouraged to place their orders this week to avoid running out.
In the lead-up to Christmas, pharmacy processing times may take a little longer than usual because of the volume of prescriptions.
Patients in North Lincolnshire should order their repeat prescriptions as soon as possible – allowing pharmacies at least 3 working days to administer.
Dr Nigel Wells, Executive Director Clinical and Care Professional for Humber and North Yorkshire Health and Care Partnership, said: “If you order your repeat medication directly via your GP Practice, please be patient – GP surgeries remain exceptionally busy at the moment.
“The easiest and quickest way to order your repeat medicine is via the NHS App, or GP Online Services – you can do this from the comfort of your own home, without having to leave the house.
“Before you order repeat prescriptions, please check what medicines you already have at home and only order the items that you need and please do not stockpile medicines. Excess supplies of medicines at home can be dangerous and is also wasteful. Once dispensed, medicines cannot be re-used and have to be destroyed.”
Keep a well-stocked medicine cabinet
Having a medicine cabinet at home with some simple over-the-counter remedies like paracetamol, ibuprofen, and anti-diarrhoea tablets is recommended so you can treat any common illnesses or ailments yourself, without needing to see a GP.
Use the right service
If it is not an emergency, you can get medical advice 24/7 by calling NHS 111 or using the 111 online service, they have trained medical professionals available who can direct you to the most appropriate medical care.
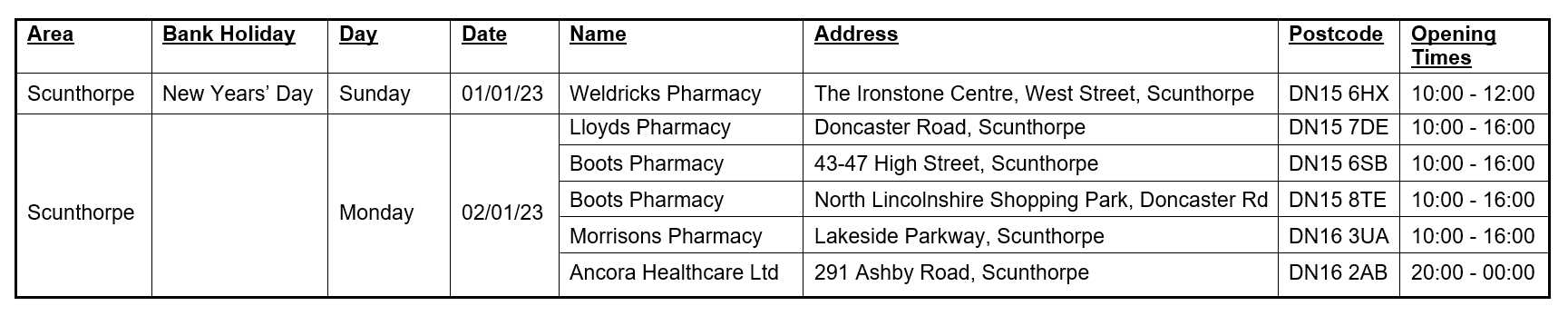
While the majority of GP surgeries are closed on Christmas Day, Boxing Day and New Year’s Day, some pharmacies in North Lincolnshire will be open and are the best place to go for help with minor health concerns.
Your local pharmacy can provide clinical advice for minor health conditions common over the winter period such as coughs, colds, sore throats, tummy trouble and aches and pains.
Please check with your local pharmacy for their opening hours, as they will vary over the Christmas and New Year period. More information can be found on the NHS website at www.nhs.uk/service-search/find-a-Pharmacy
Be aware of norovirus
Norovirus outbreaks are more common this time of year, there is no specific treatment for norovirus, but you can take steps to ease your symptoms. If you’ve got sickness and diarrhoea, stay hydrated.
Don’t see your GP unless symptoms persist more than a few days, the best ways to avoid catching norovirus is wash your hands thoroughly after using the toilet.
Look out for yourself and others
The colder weather and shorter days can affect your mental health, get out in the sunshine if you can, even short bursts can improve your mental wellbeing.
Older neighbours and relatives are more vulnerable in the winter months and may need a bit of extra help to stay well, make sure you keep in touch and check in on them when you can.
If it’s an illness or injury that is serious or life threatening, patients should always call 999 for an ambulance or go to the nearest emergency department.